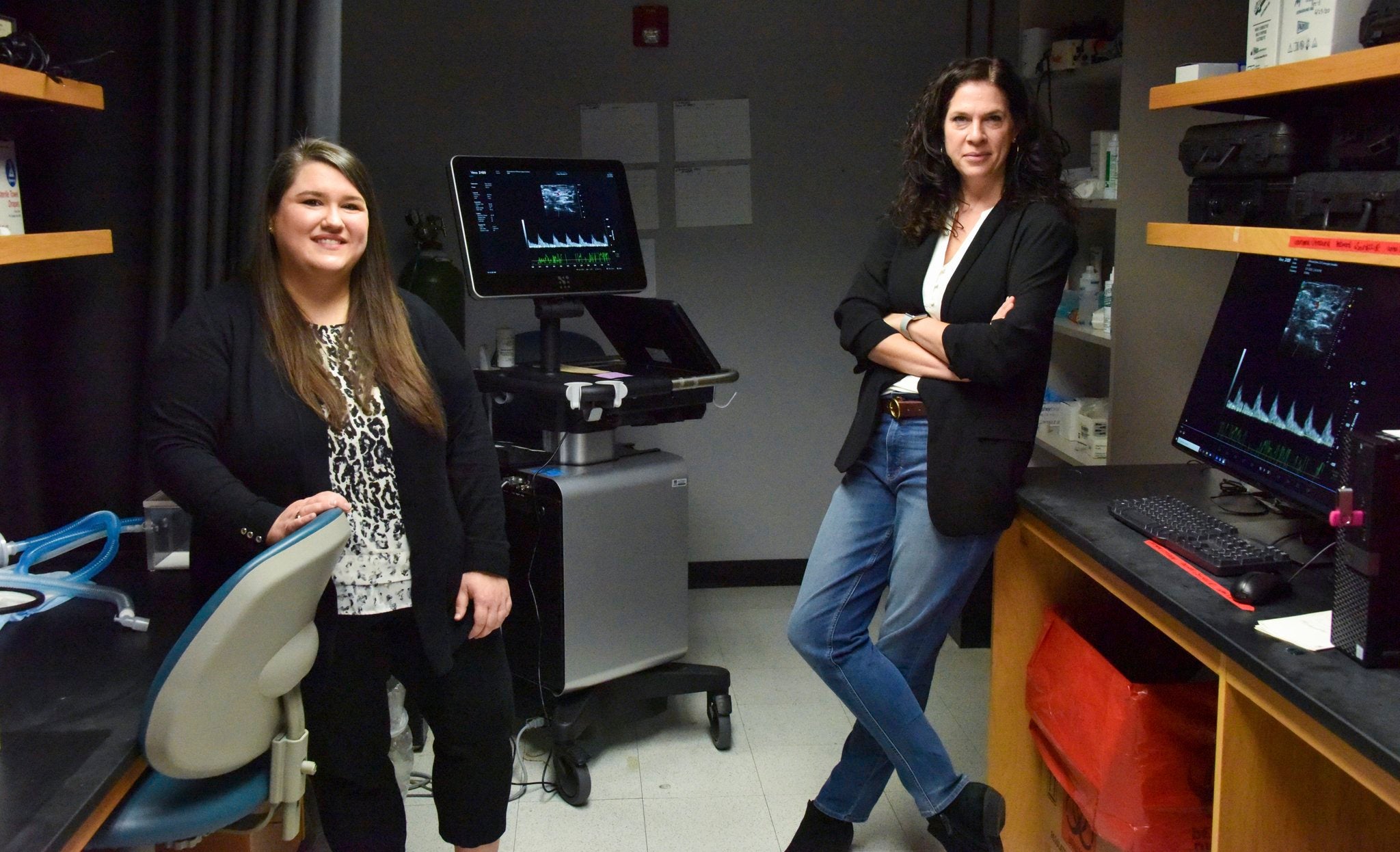
Two years of rodent-based research at the Medical College of Georgia’s Department of Physiology links previously injured kidneys to pregnancy and neonatal complications years after the organs were thought to be healed.
Results of the on-going study show young women who received treatment for acute renal injuries can later suffer pregnancy-related complications like pre-eclampsia, which is known to restrict fetal growth. Infants can experience poorer neonatal outcomes.
The findings are especially relevant since COVID-19-related incidences of acute kidney injuries are expected to increase, according to Senior Postdoctoral Fellow Ellen Gillis.
Prior to pregnancy, the patient who received kidney treatment may appear to be healthy. However, renal function increases dramatically during pregnancy, extending beyond what is typically required. Blood volume increases in order to support a growing fetus, leading to an increase in kidney function. Pregnancy is a unique physiological stressor because it presents increased demand over an extended period of time, Gillis said.
“These women, under normal conditions are doing fine,” Gillis said. “The kidney function is perfect after AKI and back to normal. However, when you have this sudden increase in demand in the kidney, then we start to see problems.”
[adrotate banner=”23″]
Two recent clinical studies found similar results to what MCG scientists found in the model they developed using rats. The rodents are a cost-effective specimen, which allows for quicker conclusions since they experience a gestation period that lasts about 23 days. Rodents and humans share mostly the same pathways during pregnancy that are altered, according to Gillis.
“Rats are a good model to use for kidney and pregnancy studies,” she said. “It’s difficult to do these studies in humans because specifically, we are interested in very early changes in kidney function in pregnancy. We can’t study humans because a lot of women don’t know early enough that they are pregnant.”
This study establishes the model of what happens, but scientists have yet to come to a full understanding of it.
“So, now is when we want to go back and look at very early stages of pregnancy to see how renal function is changing in normal pregnancies and how that is not happening in this model, “Gillis said. “We can identify what is going wrong, so that we can maybe identify a therapeutic strategy to improve outcomes for these women.”
Gillis hopes the research will ultimately allow doctors to identify risk earlier in pregnancies. Currently, conditions like pre-eclampsia and gestational hypertension are not detected until approximately 20 weeks into fetal development and only after symptoms occur.
The results of the MCG study were published in the Journal of the American Society of Nephrology.
Shellie Smitley is a staff writer for The Augusta Press. Reach her at shellie@theaugustapress.com
[adrotate banner=”44″]