Two new National Institutes of Health grants, totaling $5.7 million, are aimed at helping scientists at the Medical College of Georgia (MCG) at Augusta University better understand the mechanisms of two cardiovascular complications associated with HIV.
Thanks to a combination antiretroviral therapy (cART), which uses a combination of three or more drugs to stop the virus from replicating in the body, life expectancy of people living with HIV has dramatically increased, according to a press release from MCG.
“In fact, most people living with HIV no longer die from the opportunistic disease but instead from cardiovascular disease,” stated a press release from MCG.
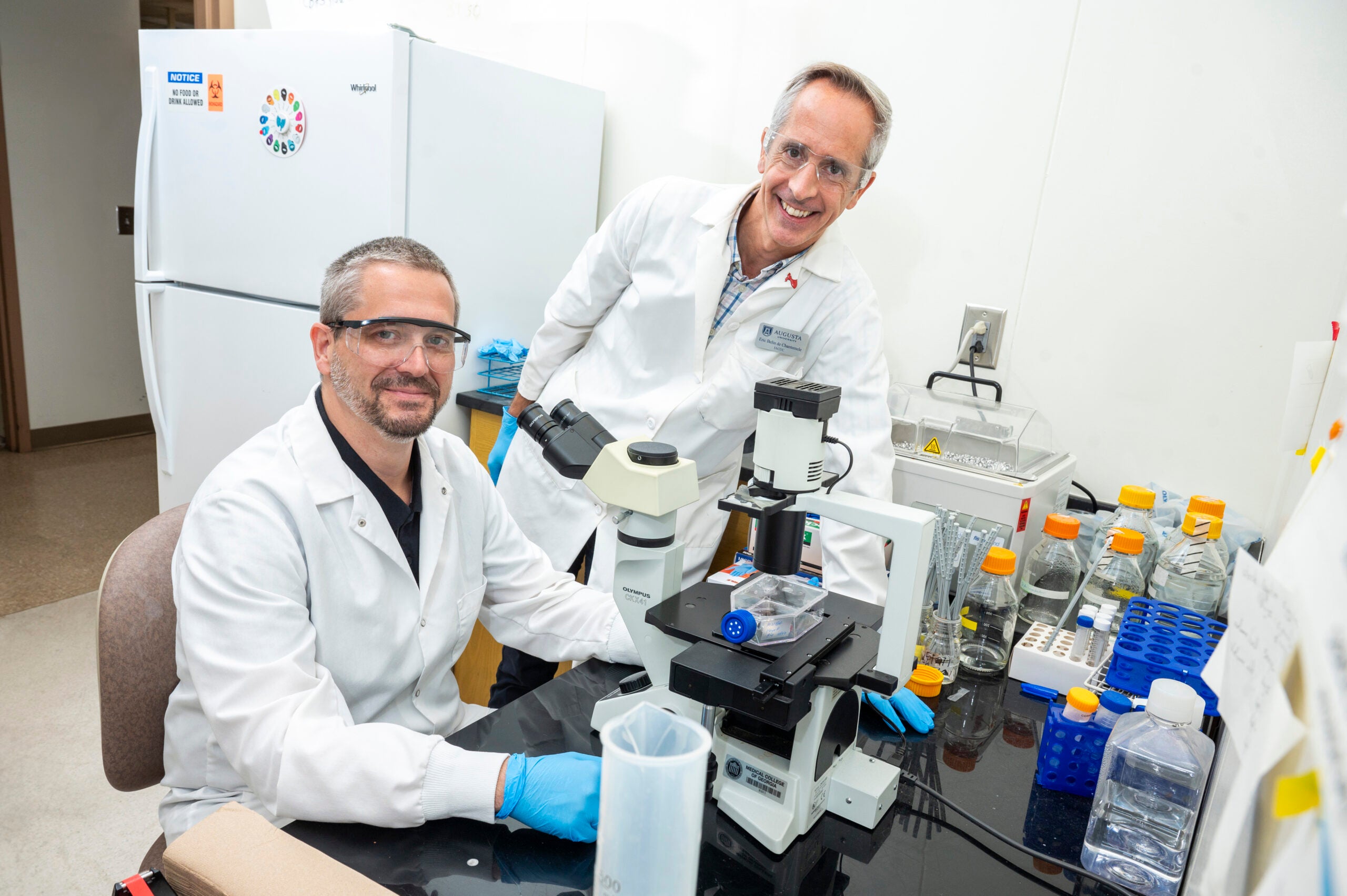
Eric Belin de Chantemèle, a physiologist in the MCG Vascular Biology Center, is the principal investigator on a new $2.7 million grant from the National Institutes of Health to help better understand why people living with HIV experience an earlier-than-normal onset and higher prevalence of hypertension, the leading risk factor for cardiovascular disease.
He theorized that HIV-derived proteins that remain in circulation, despite cART treatment and a well-controlled viral load, are contributing factors.
In a transgenic, or genetically modified mouse, model of HIV, Belin de Chantemèle has been able to show these proteins increase circulating Interleukin-1 alpha (IL-1 alpha), which plays a key role in the body’s immune response and inflammation.
“That in turn impairs endothelium-dependent relaxation, essentially how our blood vessels relax, which leads to hypertension,” according to a press release from MCG.
Inhibiting T cell activation in the mouse model resulted in restored blood pressure and improved function of vascular endothelial cells, which line the inside of blood vessels and are essential to circulation.
With this new funding Belin de Chantemèle wants to see if his findings continue to hold true.
“We also have evidence that IL-1 alpha itself accelerates vascular aging and promotes hypertension by promoting excessive reactive oxygen species, which is damaging to vascular endothelial cells,” he said.
Belin de Chantemèle and Laszlo Kovacs, from the MCG Department of Pharmacology and Toxicology, are also principal investigators on another new $3 million grant to study one of the most devastating cardiovascular complications of HIV – pulmonary vascular disease (PVD), which affects the blood vessels in the lungs.
From their research, they hope to better understand the “how and why” behind the structural changes in the walls of pulmonary arteries that are a hallmark of this disease.
“They theorize that those still-circulating HIV-derived proteins are also a root cause of that remodeling,” according to a press release from MCG. “They have early evidence that this is the case and have identified at least one of those proteins as a new marker for the development of PVD.”
Early data from three different animal models of HIV have shown that CD4+ T cells, or “helper cells” that assist the body in fighting off infection, and Podocan-like protein 1 (Podnl 1), which has been linked to the immune response in cancer, play a role.
“We also demonstrated that the expression of HIV-derived proteins in transgenic mice promotes the remodeling of pulmonary arteries, increased right ventricular systolic pressure, increased size of the heart’s right ventricle and decreased pulmonary artery acceleration time, as well as an increase in circulating IL-1 alpha,” all signs of the disease, Kovacs said.
Kovacs also said he and Belin de Chantemèle found the alterations are “exacerbated by aging.”
When wild-type mice were treated with a bone marrow transplant from the transgenic mice, with HIV, they also developed the same cardiopulmonary complications, which also supports a role for these viral proteins in the development of PVD, Kovacs said.
Using RNA sequencing, the scientists were able to specifically identify Podnl1 as a new biomarker for PVD because its levels were increased in the lungs of both the wild-type and transgenic mice and in tissue samples of people with HIV who were on cART.
“The ultimate goal is to understand how HIV-encoded proteins derived from T cells interact with lung vascular cells to promote Podnl1 overexpression and pulmonary artery remodeling,” Belin de Chantemele said. “We anticipate that both of these proposals will lead to the identification of new therapeutic targets to prevent this accelerated development of cardiovascular disease.”