Editor’s Note: This is the first part of a two part series on LGBTQ+ health issues. The story focuses on the relationship between chronic stress and the high incidence of cardiovascular disease among the LGBTQ+ community.
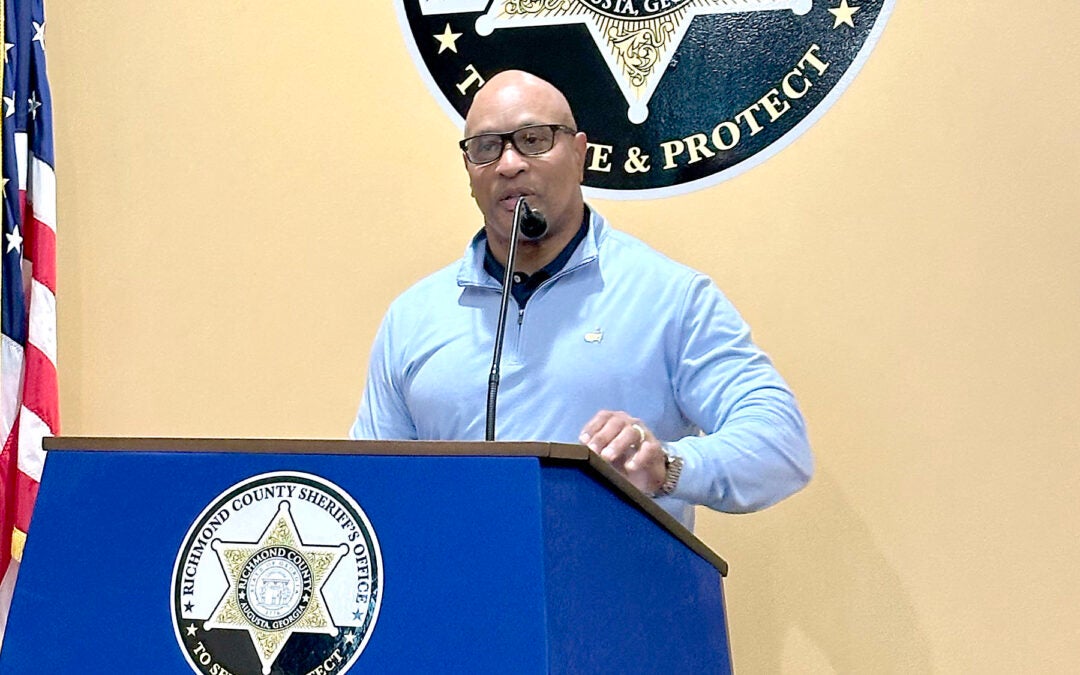
Rick Lassiter says he never stresses about anything.
“It’s not in my nature,” he said. “I watched my mother stress over things she couldn’t control.”
Rick Lassiter is one of the lucky ones.
Lassiter is a 62-year-old gay Augusta man, a native of Macon, and he grew up in a loving and supportive family who have always accepted him for who he is.

Lassiter’s experience is far different from that of many in the LGBTQ+ community who, instead, face rejection, isolation and violence, and who, consequently, live with constant anxiety, constant fear, constant stress. So much so that members of that community have a far greater occurrence of cardiovascular disease than the broader community, according to the American Heart Association.
Members of the LGBTQ+ community have more heart issues than others, according to a study published in the November 2020 issue of the medical journal “Circulation.” That is because they face health disparities due to social stigmas, discrimination and denial of civil rights, the Heart Association says.
It may be hard for non-minority people to imagine living with chronic stress so intense and unrelenting that it can lead to cardiovascular disease, but that is the reality for many who are gay, lesbian, transgender, bi-sexual or questioning – especially women who are fall into sexual minorities, according to the 2020 study.
Even harder to imagine — what if one of the sources of that stress is a health care provider – the very person whose job it is to help people achieve and maintain their health?
Augusta health care providers and researchers are well aware of the unique barriers LGBT people face when it comes to medical care. Some are even working to improve medical education so that aspiring health care workers are better prepared to treat LGBTQ+ patients.
[adrotate banner=”22″]
The first step is understanding why LGBTQ+ patients are different from others. One important difference is chronic stress, which is common among the LGBTQ+ community, according to the American Heart Association.
The body’s reaction to stress is meant to be protective, but if stress is chronic, it can threaten health.
Long-term, chronic stress increases both inflammation in the body as well as the level of cortisol. Inflammation can lead to high blood pressure and high levels of “bad” cholesterol. Cortisol is a hormone that increase cholesterol and blood pressure, both of which are known to be risk factors for cardiovascular disease, according to Tracy Casanova, an Augusta University psychologist in the Department of Psychiatry and Health Behavior. Casanova is an expert in trauma in the LGBTQ+ community as well as military sexual trauma.
“Think about most people,” Casanova said. “They experience stressors, but their stress goes down because it’s not constant. For this [the LGBTQ+] community, they can’t get away from the stress because they can’t remove their identity. The threat of identity-based trauma and discrimination does not go away.”
Those in the LGBTQ+ community worry about being rejected, and many internalize negative homophobic stereotypes. That sort of chronic stress can lead to problems with the cardiovascular system, according to the American Heart Association.
“In terms of LGBT individuals, both male and female have higher incidence of heart disease,” said Augusta University physiologist David Stepp.
Stepp holds the Leon Henri Charbonnier Endowed Chair in Physiology at AU and is associated with the Vascular Biology Center. He is a founder of Augusta Pride.
According to Stepp, LGBTQ+ individuals have the same risk factors for cardiovascular disease as the rest of the society, hypertension being among the most common.
LGBTQ+ people “don’t really manifest that differently,” he said. “What’s different, in a sense – it’s all environmental factors. We all come into this world with the cards we’re dealt.”
Those in the LGBTQ+ community have “a number of factors that contribute to overall poor outcomes,” however, Stepp added. Among those is that unrelenting chronic stress that grows out of fear and anxiety about social responses to their differences.
Many in the LGBTQ+ community deal daily with that sort of chronic stress, and a majority within that community have experienced discrimination by at least one health care provider.
While society may be more accepting of LGBTQ+ today than in the past, the same cannot be said for minority communities where transgender individuals especially face a high threat of rejection or violence, said Matt Kridel, an Augusta University psychologist and postdoctoral fellow.
“While I think there are certain stressors that have decreased for LGBTQ+ youth and LGTQ people in general, it doesn’t mean that stressors are gone entirely,” Kridel said. “LGBTQ+ people still experience discrimination, especially in more rural and conservative areas.”

Stepp agrees. He says the source of stressor among the whole LGBTQ+ community is nuanced and dependent on a number of factors. Homelessness, for example, is more prevalent among LGBTQ+ youth, and that can lead to a whole host of socioeconomic stressors, Stepp said.
LGBTQ+ youth make up 7 percent of the 4.2 million young Americans, but they account for 40 percent of homeless youth, according to statistics from True Colors United, a non-profit that serves homeless LGBTQ+ youths.
Alan Braden, a member of Augusta Pride who runs the annual parade, did the research for his master’s degree on homeless LGBTQ+ youth. He said his research showed homelessness among LGBTQ+ youth commonly results from being thrown out of their homes by family members who reject them for their sexuality or who are forced to flee due to violence at home.
Being homeless as a young person often means having less education, and a lack of education impacts job opportunities, Braden said. Low-paying jobs often mean one has to deal with poverty, which presents its stressors.
That discrimination presents in a variety of forms — violence, hate language, eviction, loss of employment or denial of services, Kridel said.
“For people with multiple marginalized identities, these stressors are even worse,” he added. “Trans women of color are significantly more likely to experience violence or be murdered than any other group.”
Transgender individuals especially face rejection and isolation, according to AU psychologist Tracy Casanova. Physical differences make them more visible, thus more vulnerable to discrimination because of the greater stigmas attached to being transgender.
Stepp says socioeconomic stress, in addition to discrimination by medical personnel and others, is implicated in cardiovascular health issues among LGBTQ+ adults.
“You can’t get jobs in certain environments, you’re pressured to leave school through family or peer pressure – the same things that effect all minorities are just as prevalent in the gay community,” Stepp said.
[adrotate banner=”29″]
Echoing the AHA, Stepp added that there is tremendous social pressure when someone is both LGBTQ+ and a member of a rejected minority. Many respond to that stress by using illegal drugs and alcohol or smoking.
HIV and AIDS are other stressors for some in the LGBTQ+ community. Although being HIV-positive is no longer the death sentence it once was, due to new treatments, being HIV-positive is still a stressor in-and-of-itself.
“I don’t want to say HIV causes heart disease, but maybe there’s a predisposition” among those who test positive or are in treatment for the disease, said Cheryl Newman, a physician who specializes in treating HIV patients.
The mechanism could be chronic infection, it could be chronic inflammation. Both can contribute to cardiovascular disease, Newman added.
So, while HIV isn’t directly linked to cardiovascular disease, the two are at least loosely linked. That link may be a result of the medicines used to treat HIV, or it may that the drugs can cause weight gain—or it could be coincidental, Newman said.
Ultimately, the stressors LGBTQ+ people face all focus on their identities, even HIV, which is intimately tied to the gay male community in particular, though not everyone infected with HIV is gay or male. Identity-based stress is the most severe kind of stress there is, Kridel said. Members of that community often have to deal with landlords who refuse to rent to someone who is gay or trans, employers who will fire gay or trans employees, health care providers who refuse to treat gay or trans patients.

“All of those kinds of stressors can be deleterious on someone’s health,” Kridel said. “A compounding effect occurs over time, and it can show up as heart disease or a lowered immune system.”
Braden agrees.
“When you’re constantly afraid of being your genuine self, you can’t operate at your best,” he explained.
Braden says he has experienced the stress that comes with being openly gay. He moved to the Augusta area a number of years ago to help care for his mother, his car had a rainbow sticker on it. His mother encouraged him to scrape the sticker off his car “before someone puts a brick through a window,” he said.
“There are still a lot of conservative views in this town that can work against you in employment,” he said. “There are also issues in housing. It’s not until you show up with your significant other that people realize. There are no real protections out there.”
Maybe “at the very highest altitudes” of society people have started to connect the Civil Rights Act with sexual orientation and gender identification, but that has not “trickled down to the ground level,” Braden added. At 56, he doesn’t anticipate that trickle-down occurring during his lifetime.
Stress causes cardiovascular health problems in several ways, particularly when the stress is chronic, say local physicians.
“When you have chronic stress, then when you are exposed to a stressor or new condition, you will react more than other people,” Gaston Kapuku said. “Your blood pressure will go up more than other people’s. Your heart rate will get fasters. Your arteries constrict.”
Kapuku is a cardiologist at Augusta University’s Georgia Prevention Institute. He studies the effects of stress on those who are predisposed to heart ailments.
This reaction to stress could predispose someone to congestive heart failure or other cardiovascular illnesses, according to Kapuku. That is the kind of stress those in the LGBTQ+ community experiences.
“They are pretty much in a constant situation where they have to adapt so they can be accepted,” he explained. “There really is no time for their cardiovascular system to rest. That is not good for the cardiovascular system.”
Stress can have an effect of blood vessels by causing them to constrict, or it can cause the heart to pump faster, according to Kapuku.
[adrotate banner=”23″]
When stress causes blood vessels to constrict, they cannot deliver blood to the organs as efficiently. When organs are deprived of blood, they age faster, Kapuku said. A faster beating heart is likely to cause disease because it pumps faster for a period of time and then declines back to normal, he added.
Minorities, whether sexual or racial, tend to have vascular reactions more than the majority community. Consequently, the gay community and the Black community have similar problems with their arteries constricting in response to stress, he added.
This is because majority communities have a sense of mastery or control over their lives, Kapuku explained.
“Studies are showing that being a minority gets you to the point where you lose your mastery, the control over your life,” Kapuku said. “The sense of control is minimized in a community that feels discriminated against.”
Kapuku says it is important to address stress within the LGBTQ+ community.
“We have to start addressing it,” he said. “We can’t go on as a society ignoring an important part of our community. It would be like ignoring the Black population.”
Kapuku would like to see medical schools address the care of the LGBTQ+ population. That way, young physicians would go into the workplace armed with appropriate knowledge to help them diagnose and treat sexual minorities. He thinks a broader humanities education would be one way to improve how practitioners treat LGBTQ+ patients.

When treating Black patients, physicians know that they have to treat hypertension differently than in the white community, he said.
“The LGBTQ+ community needs that kind of knowledge,” he added.
Vishal Arora, also a cardiologist and a member of the Augusta Heart Association board, agrees. He says that more than half of those in the LGBTQ+ community have experienced some form of discrimination, mostly in the form of verbal abuse, from their medical providers.
“Doctor-patient relations are based on trust,” Arora said. “If you don’t trust your provider, you’ll be less likely to seek their help when needed.”
The biggest problem with that lack of trust is a delay in seeking treatment, he added. Better preparation in medical school, an enhanced curriculum, for example, could help doctors become more aware of the health challenges specific to the LGBTQ+ community.
“We need to educate and equip health care providers to be more compassionate and caring,” he said.
Arora encouraged those in the LGBTQ+ community not to be afraid to move on to another doctor if one isn’t meeting the patient’s needs.
Providers can also treat the stress itself. Sometimes, one of the best treatments for those in the LGBTQ+ community is simply having someone to list to their fears and concerns, Kridel said. Once they know they’ve been heard, some are ready to move forward with learning how to recognize and deal with stressors.
Self-acceptance and personal strength are sure factors that will help anyone deal with stress, said both Kapuku and Casanova.
“Knowing it’s ‘them’ and not you,” combined with community support can help an individual achieve resiliency, said Casanova.
Lassiter is an example of that resilient personality Casanova talked about. He says he never stresses about anything.
[adrotate banner=”19″]
Lassiter says he always tells his health care providers that he’s gay because his lifestyle could affect his health. He says he’s never had anything but positive experiences with health care providers – with one minor exception when he and a nurse got into a tiff about who was going to stick his finger to draw blood. He wanted to do it himself so he could stick the side of his finger instead of the fingertip.
“It wasn’t a bad experience. Just a little strange,” he said.
Lassiter has never really been rejected by anyone for his sexuality, he said.
“I never had any issues with my parents. My siblings, less so, and my nieces and nephews were less of a problem. Even less a consideration for my great-nieces and -nephews,” he said. “I think it’s generational.”
Lassiter was adopted and that his mother knew he was gay from the time he was a small child, he said. If anyone had a problem with him being gay, they also had a problem with his mother, who was his staunchest ally. He recalled the time a woman at his childhood church was moving toward calling homosexuality a sin in a conversation with his mother. Before she could, Lassiter’s mother stopped her, grabbed his hand, and declared, “Every mother should be blessed with a gay son.”
“You can listen to someone all day and give them cognitive and behavior strategies, but that isn’t going to change fact that they’re being discriminated against,” Kridel said. “It still requires advocacy from health care providers at local and other levels” to address LGBTQ+ health care and discrimination.
Sometimes, health care providers are the best advocates simply because of the credibility they have in most communities.
“Medical professionals hold a lot of power and thus have a lot of power to advocate for those changes,” Kridel said.
The way medical professionals interact with LGBTQ+ patients can also influence how stressful treatment can be. That will be the subject of tomorrow’s story in this series.
Debbie Reddin van Tuyll is Editor-in-chief of The Augusta Press. Reach her at debbie@theaugustapress.com.
[adrotate banner=”50″]